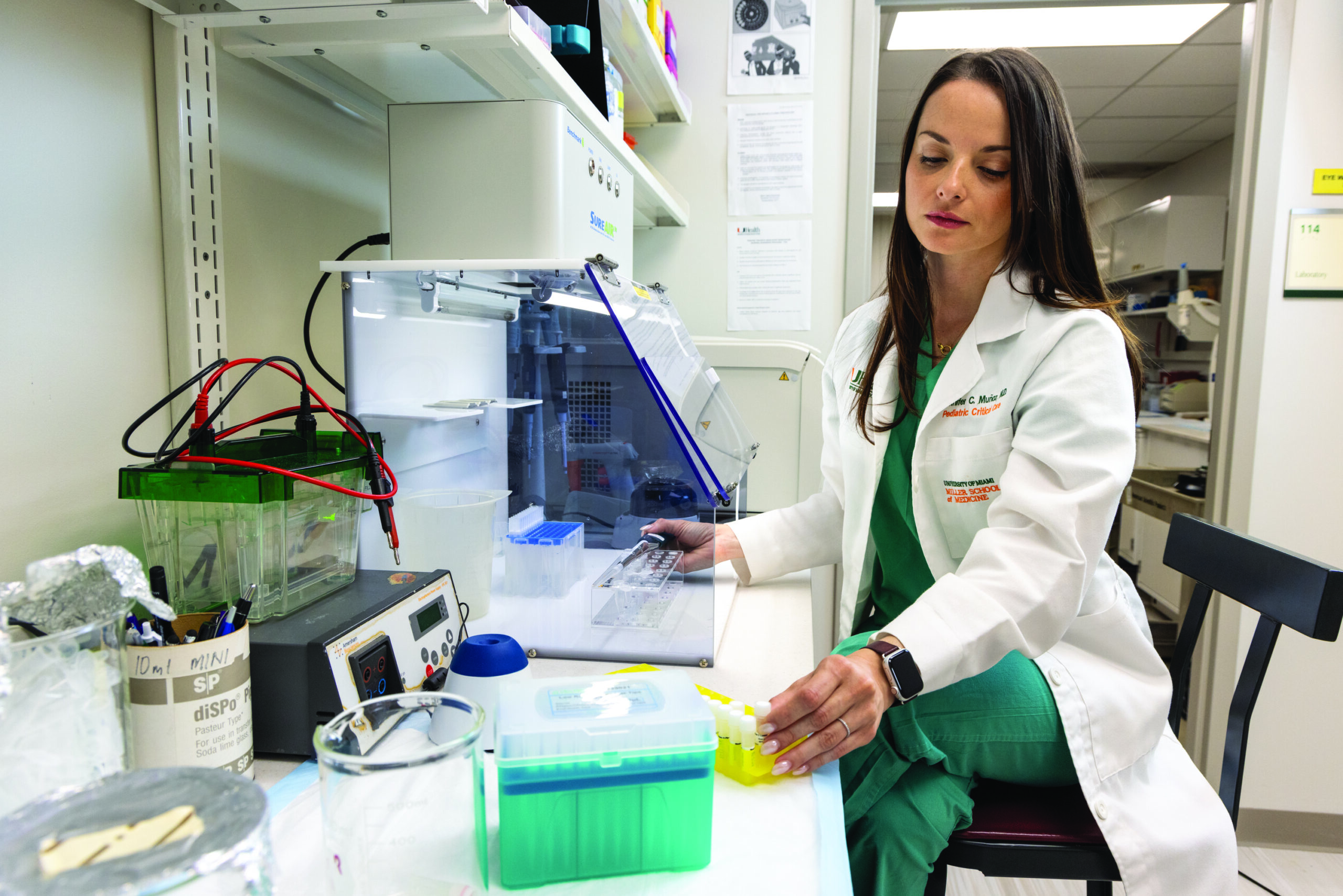
Jennifer C. Munoz Pareja, MD, Associate Professor Division of Pediatric Critical Care, interim Section Chief of Pediatric Cardiac Critical Care and Associate Program Director of the Pediatric Critical Care fellowship program at Holtz Children’s Hospital, joins The Miami Project to Cure Paralysis to hone proven neuroscientific excellence onto the topic of pediatric critical care. Her demonstrable experience and expertise with biomarkers for neurological conditions in the pediatric intensive care setting now unites with The Miami Project’s expertise in neurologically relevant biomarkers to shape a vision for the future of pediatric critical care.
Born and raised in Colombia, Dr. Munoz Pareja’s early fascination with aerospace medicine propelled her towards a career dedicated to healing and discovery. During medical training in her home country, the William J. Harrington program enabled her to spend time at Jackson Memorial Hospital linking training to the University of Miami Leonard M. Miller School of Medicine and Jackson Health Systems. This invaluable experience paved her way to a career in the united States. Soon after graduating from medical school at only 20 years of age, she moved to Miami and completed a pediatric residency at Nicklaus Children’s Hospital and a subsequent fellowship in Pediatric Critical Care at Harvard Medical School / Massachusetts General Hospital. During her fellowship, she was mentored by Dr. Ann-Christine “Tina” Duhaime, MD, Chief of Pediatric Neurosurgery, solidifying her interest in acute brain injury. Soon after in her appointment at University of Florida College of Medicine, she honed her neurological interests under the training of Kevin K. Wang, PhD, well known for their biomarker research as a site of the NINDS-funded, multicenter Transforming Research and Clinical Knowledge in Traumatic Brain Injury (TRACK-TBI). Dr. Munoz Pareja now moves to the Miller School to conduct biomarker and neuroinflammation research in acute brain injury after pediatric critical care illness. She does so while maintaining a practice of excellence in pediatric critical medicine and contributing to the training of the next generation of physicians in her specialization.
With her vision informed by this rich experience, Dr. Munoz Pareja now joint the University of Miami to unite her clinical acumen with The Miami Project’s scientific affordances. Her trajectory demonstrates she has realized the potential of fluid biomarkers in the pediatric clinical care setting, and tapping into The Miami Project will unlock a deeper understanding of the underpinnings of pediatric acute brain injury, revolutionizing the diagnosis and treatment of this understudied condition in the pediatric population.
Her groundbreaking work, highlighted in a recent paper published in Journal of Neurotrauma titled “Prognostic and Diagnostic Utility of Serum Biomarkers in Pediatric Traumatic Brain Injury”, showcases the potential of this union. The study analyzed biomarkers like GFAP, tau, S100B, and p-tau181 in blood to predict TBI severity and long-term neurological outcomes. The results of the study suggest that a specific panel of blood biomarkers, a bodily fluid already readily and routinely accessed in this situation, at key points after TBI can aid in earlier diagnosis and more granular prognosis compared to current standards. This study emphasizes the power of uniting Dr. Munoz Pareja’s visionary mindset with The Miami Project neuroscientific expertise, notably the fluid biomarkers expertise of Dr. Juan Pablo de Rivero Vaccari, to understand acute brain injury after critical illness and inform subsequent care. This study not only informs clinical decision-making now, but the approach also holds the promise of identifying novel therapeutic targets for TBI and other neuro critical conditions. This multidisciplinary approach to pediatric medical research, leveraging advanced technologies like Dr. de Rivero Vaccari’s Simoa HD-X empowered biomarkers core that she helped advocate for, epitomizes the potential afforded by Dr. Munoz Pareja bringing pediatric medical research to The Miami Project. The future will include the deep dive into TBI but also include nontraumatic brain injury especially those from hemodynamic dysfunction since these causes of brain emergencies are not readily diagnosed radiologically thus warranting fluid biomarker efforts. Already she has launched a project in children with congenital heart disease, studying neuronal injury biomarkers and neuroinflammation after cardiopulmonary bypass at Holtz Children’s Hospital. In addition, she plans to continue previous collaborations to study another nontraumatic neurological condition in the form of childhood delirium with Dr. Amanda Alladin at the University of Miami and Dr. Chani Traube at Cornell University.
In addition to her research endeavors, Dr. Munoz Pareja is an active leader in her field and, while also still in many ways at an early phase of her career, already passionate about training the next generation in a truly global context. For the Neurocritical Care Society, she is currently the co-chair of the Emergency Neurological Life Support and has developed a pediatric neurocritical care simulation curriculum for variable resource settings with international collaborators that will enable training in areas such as Africa and Latin America. In addition, she is also a co-chair of the Pediatric Neurocritical Care Research Group global health committee, advocating for excellence in pediatric neurocritical care across the globe. Locally, she is the Associate Program Director of the Pediatric Critical Care fellowship program at Jackson Health System’s Holtz Children’s Hospital, where she shapes the next generation of pediatric critical care physicians. Her Florida ties also keep her linked to the state’s pediatric TBI consortium, which she founded in 2017.
So it is that Dr. Jennifer C. Munoz Pareja’s visionary approach to academic medicine unites with The Miami Project’s neuroscientific expertise to bring pediatric critical care to new heights.